Researchers from Caltech have developed a wearable microfluidic biosensor, dubbed Stressomic, that can monitor stress hormones such as cortisol, epinephrine, and norepinephrine in sweat.
Electrochemical assays and human studies demonstrated that Stressomic reliably tracks hormone fluctuations in response to physical, psychological, and pharmacological stressors.
Wei Gao – Professor of Medical Engineering and corresponding author of the study – and his team have spent years advancing wearable biosensors and microfluidic platforms for monitoring metabolites, electrolytes, and hormones in sweat and other biofluids. “When we realized that our microfluidic and electrochemical approaches could, in theory, push the detection limits low enough to measure catecholamines like epinephrine and norepinephrine – at picomolar levels – that opened up a completely new space for stress research,” says Gao.
He also recognized a clear unmet clinical need. “Stress is a major driver of mental and physical health problems, yet current assessments are often subjective or indirect,” he says. “We saw a gap in the ability to continuously and noninvasively monitor the body’s actual biochemical stress signals, especially in real time.
The device uses iontophoresis to extract sweat and bursting valve-regulated microfluidic channels for continuous sampling and analysis, which is done via laser-engraved graphene electrodes – achieving picomolar-level sensitivity. Watch the in-vitro flow test here.
“When we actually confirmed the presence of epinephrine and norepinephrine in sweat at physiologically meaningful levels – it was a real ‘we can actually do this!’ moment, since this hadn’t been shown in situ before,” says Gao.
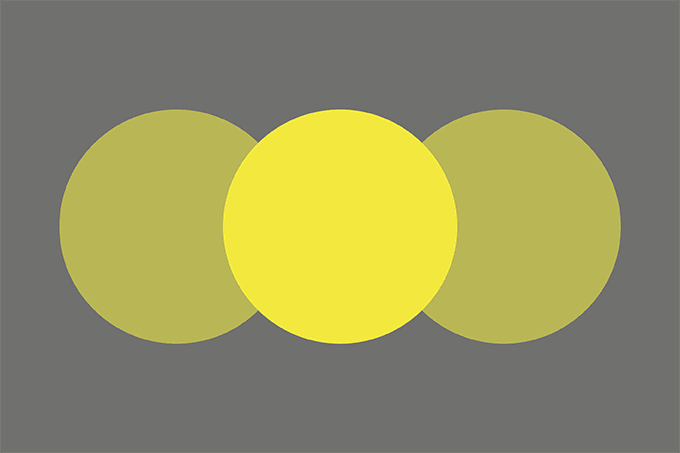
The researchers also uncovered some interesting hormone dynamics in response to stress. Emotional stress, which they induced by showing participants a series of “emotionally provocative images assisted by auditory stimuli” barely moved cortisol but clearly elevated norepinephrine. Whereas physical stress – participants followed a HIIT protocol on a stationary bike – boosted both cortisol and norepinephrine.
“That reinforced how different stressors engage different arms of the stress response, and it made us realize how much nuance you miss if you only track one hormone,” says Gao.
In 2014, The Analytical Scientist reported on a smart mask, developed by Gao and his colleagues, to monitor breath biomarkers in real time – but that dealt with analytes at relatively higher concentrations. “Stressomic was like working with a whisper instead of a shout,” says Gao. “Catecholamines are present in sweat at extremely low levels – picomolar. That meant we had to engineer both the sensing interface and the microfluidics to maximize sensitivity, specificity, and temporal resolution.”
The gold nanodendrite–decorated laser-engraved graphene electrodes gave the researchers the sensitivity boost, and the microfluidic module – with capillary burst valves – let them take time-stamped “snapshots” of sweat composition without signal washout. The team also had to balance incubation time (needed for the immunoassay) with the rapid changes in hormone levels. “Our sequential chamber design helped align those time scales,” says Gao.
Potential applications span from clinical monitoring of stress-related disorders to performance optimization in athletes, astronauts, or military personnel. It could also be a tool for mental health research, helping to link physiological and psychological states.
But is there a risk that tracking stress markers actually increases stress? “It’s a fair point,” says Gao. “We think the key will be in how the data is presented. If it’s framed as supportive feedback – like heart-rate zones for exercise – users can learn their patterns and triggers in a constructive way. But raw numbers without context could indeed be anxiety-inducing, so user-centered interface design will be crucial.”
In terms of next steps for Stressomic, the researchers are now moving in “three directions at once.”
“We want to demonstrate real-world wearability: miniaturizing the electronics further, improving battery life, and making the patch more comfortable for long-term use,” says Gao. “We’re also expanding the biomarker panel: adding inflammatory and metabolic markers to put stress responses in a broader physiological context. Finally, we’re partnering with clinicians to test the system in patient populations with anxiety disorders, PTSD, or chronic stress, and to see how it can guide personalized interventions.”
Gao also emphasized the importance of interdisciplinary collaboration for the research.
“The project brought together expertise in electrochemistry, microfluidic engineering, flexible electronics, wireless communication, and human physiology,” he says. “Within my group, we had team members focused on electrode surface chemistry, others on laser-patterned microfluidics, others on firmware and data processing. We also collaborated with chemical engineers for microfabrication strategies and with physiologists to design the human studies.”
“Without that mix of skillsets – and a lot of whiteboard problem-solving sessions – this system wouldn’t have come together.”