What is your goal?
My research group focuses on translational research and clinical imaging. My main interest is to provide new clinical diagnostic tools, with a focus on intraoperative diagnostics. Therefore, I am strongly connected with the hospital and working very closely with surgeons and pathologists. Our ultimate, joint goal is to improve the clinical decision-making process (surgical and medical) that results in better patient outcome. This is what drives me and my research.What problem do you hope to solve?
Surgery is the best hope of a cure in 80 percent of diagnosed cancer cases. Whether a cure can be achieved usually depends on the quality of the surgical resection (removal) of the tumor. At the moment, it is hard for surgeons to find the edges of the tumor and remove all the cancerous tissue. To find out if any cancer remains, frozen cut tissue sections are evaluated by a pathologist; results are often not available for several days, and sometimes prove inconclusive. There is ample evidence that improving the accuracy of surgical resection would reduce the number of patients requiring further surgery and improve overall outcomes. This is where molecular profiling based on mass spectrometry comes in – by using a tissue (disease)-specific database we can provide real-time and specific molecular analysis of tissue and assist the surgical decision-making process. We can also use rapid molecular pathology of resected tissue to assist pathologists in their diagnosis.Tell us about the iKnife…
The technology behind “iKnife” or “intelligent scalpel” is rapid evaporative ionization mass spectrometry (REIMS). – developed by Zoltan Takats for the rapid classification of human tissue via MS analysis. It analyses aerosols released during electrosurgical dissection using electric scalpel or forceps. The smoke generated during electrosurgery is very rich in molecular information, including tissue-specific profiles that discriminate between the tumor and surrounding tissue – data not available to the naked eye of the surgeon. The electrosurgical aerosol collected in real-time is compared with a reference model to determine (within seconds) the type of tissue being cut (for example, tumor versus non-tumor). In a clinical setting, the data would be provided interactively to the surgeon as they cut the tissue. Through this rapid, on-line analysis, surgeons get immediate feedback to help them resect the tumor accurately, leaving no cancerous tissue behind. The beauty of this approach is that existing surgical devices need no modification to combine them with REIMS, the surgical procedure remains the same, and surgeons need no extra training. And for me, these are key points to accelerate the translation of the technique into clinical practice. Currently, reference models are built ex vivo, which permit the creation of spectral databases for prospective use. In Maastricht, we are currently building databases on breast, colorectal liver metastasis, sarcomas, and head and neck tumors, which are validated histologically by expert pathologists. Our next step is to move our work in vivo and go into the operating theatre, where we will work closely with the clinical staff and surgeons. The goal is to validate the databases that we are currently building ex vivo and work with clinicians towards integration of the iKnife in clinical routine.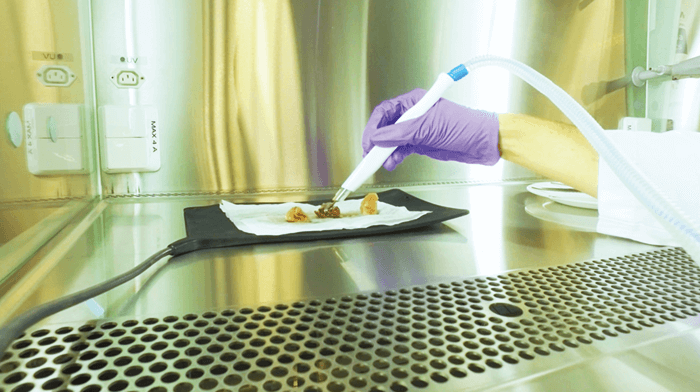
What developments lie ahead?
Recent developments have concentrated on miniaturization of the system and making it minimally invasive. For example, integration of REIMS with an endoscopic polypectomy snare to allow in vivo analysis of the gastrointestinal tract is a promising methodology to explore internal structures in a minimally invasive way (1). High diagnostic accuracy for tumor type and known histological features of poor prognostic outcome in colorectal cancer was reported, based on a multivariable analysis of the mucosal lipidome. The potential of this approach for other minimally invasive procedures has also been demonstrated by combining real-time MS with surgical laser systems where aerosol is generated by thermal ablation. The molecular patterns generated are specific to the cellular phenotypes and can easily distinguish benign from malignant regions in patient biopsies, which opens the door for applications in a wide range of clinical areas. Additionally, the cavitron ultrasonic surgical aspirator (CUSA), which is widely used for brain and liver surgery, can also be combined with the REIMS technology for intraoperative diagnostics (2).References
- J Alexander et al., “A novel methodology for in vivo endoscopic phenotyping of colorectal cancer based on real-time analysis of the mucosal lipidome: a prospective observational study of the iKnife”, Surg Endosc, 31, 1361–1370 (2017). KC Schäfer et al., “Real time analysis of brain tissue by direct combination of ultrasonic surgical aspiration and sonic spray mass spectrometry”, Anal Chem, 83, 7729–7735 (2011).