One in three people over the age of 70 suffers from peripheral artery disease (PAD), a narrowing of arteries that occurs most often in the legs. Plaque, a substance composed of cholesterol, calcium and fibrous tissue, builds up in the arteries and hardens over time, reducing blood flow. Symptoms range from pain to difficulty fighting infection and in severe cases, tissue death. Treatment with adipose-derived stem cells offers great promise for restoring blood flow, but the inherently oxygen-deprived environment causes the majority of stem cells to die before they can be of regenerative benefit.

Researchers at the University of Texas at Austin are working on a controlled oxygen delivery system to improve the survival of stem cells during treatment and thereby promote growth of new blood vessels. The teams are planning to add oxygen-saturated perfluorocarbon (PFC) nanodroplets to the hydrogel stem cell carrier destined for implantation at the treatment site. Oxygen would then be released from the nanodroplets into the surrounding tissue through passive diffusion at a rate that depends on the composition of the nanodroplet shell and the implantation environment. Additionally, a more dramatic oxygen release can be accomplished via laser “activation” of the nanodroplets. Irradiation at specific wavelengths, dependent upon absorbers encapsulated within the PFC nanodroplets, causes a rapid phase-change into a microbubble, facilitating oxygen release. This allows the location and timing of oxygen delivery to the treatment area to be controlled and tunable on a per patient basis. Laser activation can be used to control the release of oxygen from the nanodroplets into surrounding tissue. As a first step, the researchers looked at oxygen release in solution. Galvanic oxygen probes proved unsuitable, being too bulky and prone to interference from the bubbles that occurred during activation, resulting in inaccurate measurements. Instead the team chose our NeoFox optical oxygen sensor based on phase fluorimetry. NeoFox is immune to most environmental effects and can be configured with a probe that is <1 mm in diameter for use in small samples.
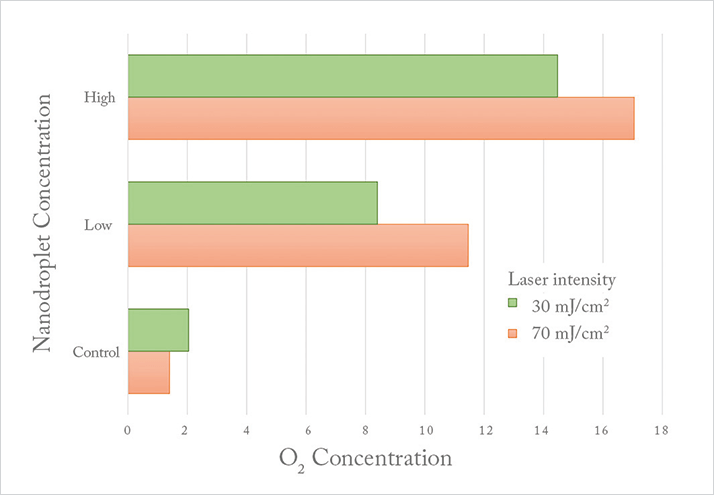
In testing, a marked increase in oxygen levels was seen for the nanodroplet-containing solutions as compared with the control, scaling with concentration. Use of higher activating laser intensity also increased oxygen release. Most importantly, the oxygen release achieved appears to be sufficient to boost oxygenation to levels that will increase implanted stem cell survival and lead to improved therapeutic outcomes for PAD patients.
The next steps for the group will be to repeat these experiments in a hydrogel format, followed by in situ tissue studies. The small size of an optical oxygen probe and its ability to work in different media will allow the team to use a single system for the full scope of research, and speed their progress in improving the effectiveness of a promising treatment for peripheral artery disease.





