A stem cell-based “disease-in-a-dish” model has uncovered a rare type of brain cell that may drive chronic inflammation in progressive multiple sclerosis, offering new clues to why the disease worsens over time.
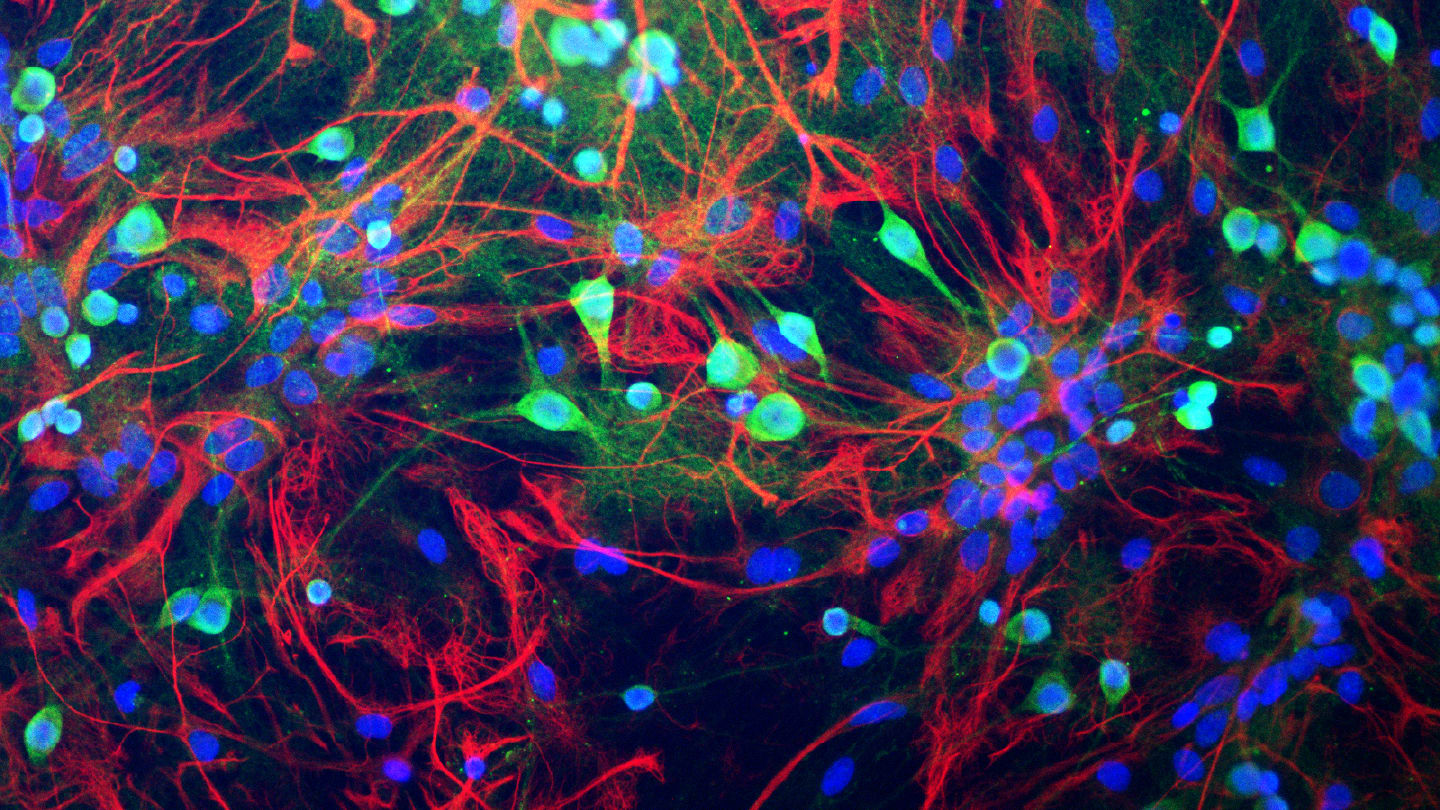
In a study published in Neuron, researchers at the University of Cambridge and the US National Institute on Aging took skin cells from individuals with progressive MS and reprogrammed them into induced neural stem cells (iNSCs), which can develop into different brain cell types. During the reprogramming process, a subset of the cells reverted to a developmentally immature state resembling radial glia – scaffolding cells found in the embryonic brain that help form neural circuits.
What set these cells apart wasn’t just their identity, but their behavior. Termed disease-associated radial glia-like cells (DARGs), they appeared six times more frequently in MS-derived lines than in controls. The cells showed hallmarks of senescence – premature aging at the cellular level – and an outsized sensitivity to interferons, molecules that play a central role in immune signaling and inflammation.
“Progressive MS is a truly devastating condition, and effective treatments remain elusive,” said Stefano Pluchino, joint senior author from Cambridge’s Department of Clinical Neurosciences. “Our research has revealed a previously unappreciated cellular mechanism that appears central to the chronic inflammation and neurodegeneration driving the progressive phase of the disease.”
“Essentially, what we’ve discovered are glial cells that don’t just malfunction – they actively spread damage,” Pluchino added. “They release inflammatory signals that push nearby brain cells to age prematurely, fuelling a toxic environment that accelerates neurodegeneration.”
Single-cell RNA sequencing and spatial transcriptomics of post-mortem MS brain tissue confirmed that DARGs cluster around chronically active lesions – regions most affected in progressive disease – often next to inflammatory immune cells, reinforcing their likely role in driving damage.
Alexandra Nicaise, co-lead author, said the team is now focused on dissecting the “molecular machinery behind DARGs” and exploring interventions to either reverse their dysfunction or eliminate them, adding: “If we’re successful, this could lead to the first truly disease-modifying therapies for progressive MS.”