Selecting the healthiest embryos remains one of the greatest challenges in assisted reproductive technologies (ART), given that nearly two-thirds of human embryo transfers fail. Current tools – from morphology-based imaging to preimplantation genetic testing – provide valuable insights but capture only part of the picture. Genetic testing, in particular, requires invasive biopsies.
Now, researchers present micro magnetic resonance spectroscopy (micro-MRS) as a powerful alternative. By applying micro-MRS to more than 150 bovine embryos and oocytes, the team showed that metabolic fingerprints can distinguish between embryos that developed successfully and those that arrested, while also correlating with oocyte maturation state. Machine learning models trained on these spectral biomarkers achieved high predictive accuracy, and multigenerational safety tests in mice found no evidence of adverse effects from magnetic field exposure.
To learn more about the origins of the work and its path from nanoliter-scale NMR microchips to embryo screening, we spoke with Marco Grisi, corresponding author and CEO and Founder of Annaida Technologies, Switzerland.

What was your main inspiration for this study?
The inspiration came during my PhD, where I developed one of the most sensitive nanoliter-scale NMR microchips yet reported. While writing this article, published in 2017, it struck me that many animals, including mammals, begin life from a nanoliter volume, and that maybe we could use this tool to study life right from its origins. What began as scientific curiosity quickly transformed into something deeper once I learned how poor current embryo selection methods are in IVF, and how distressing the journey can be for patients.
What really pushed me was a conversation with two leading embryology experts, who were already working on embryo metabolism as a marker of viability. They highlighted the unmet need for a non-invasive, reliable, and quantitative metabolic screening method. Connecting the dots: the unmatched chemical insight that MRS can provide, and the fact that I had already built a tool capable of performing MRS at these scales, I knew we had something unique. That’s when I committed to building Annaida Technologies and bringing this vision to reality.
IVF success rates remain disappointingly low – do you see metabolic profiling as the missing link in improving embryo selection?
Yes, let me explain why. Under the microscope, we see the arrangement of visible elements such as membranes or compartments, but these structures are themselves the consequence of the underlying chemical reactions that make up metabolism. It tells you what is, not what will be.
Similarly, genetic screening (mainly PGT-A) can rule out embryos with severe chromosomal abnormalities. It tells us if something essential is missing, but it gives no information about how the embryo is functioning right now. It also requires an invasive biopsy that physically removes cells from the embryo, which is especially controversial in younger patients where the benefit is marginal.
Metabolism, by contrast, is how the embryo functions. It’s the engine of development, the real-time chemistry that drives cells’ structures into place. Because metabolic changes logically precede visible morphological ones, metabolism provides the earliest and most sensitive window into embryo health.
We believe that metabolic profiling with micro-MRS can complement current methods and, in time, reduce reliance on invasive procedures like embryo biopsies. Someday, it may help us move away from what may be remembered as a rather “primitive” approach to embryo screening (have a look at this video to see what I mean).
What was the biggest analytical challenge you faced in this study – and how did you manage to overcome it?
The biggest challenge was sensitivity. Standard NMR systems aren’t designed to work at nanoliter scale; the signals are extremely weak, especially when trying to detect metabolites beyond the dominant water signal. We also had to solve for sample handling and reproducibility: embryos are delicate and keeping them positioned reproducibly during measurements was a major obstacle. On top of that, everything had to be done under strictly biocompatible conditions so that the embryos remained viable throughout.
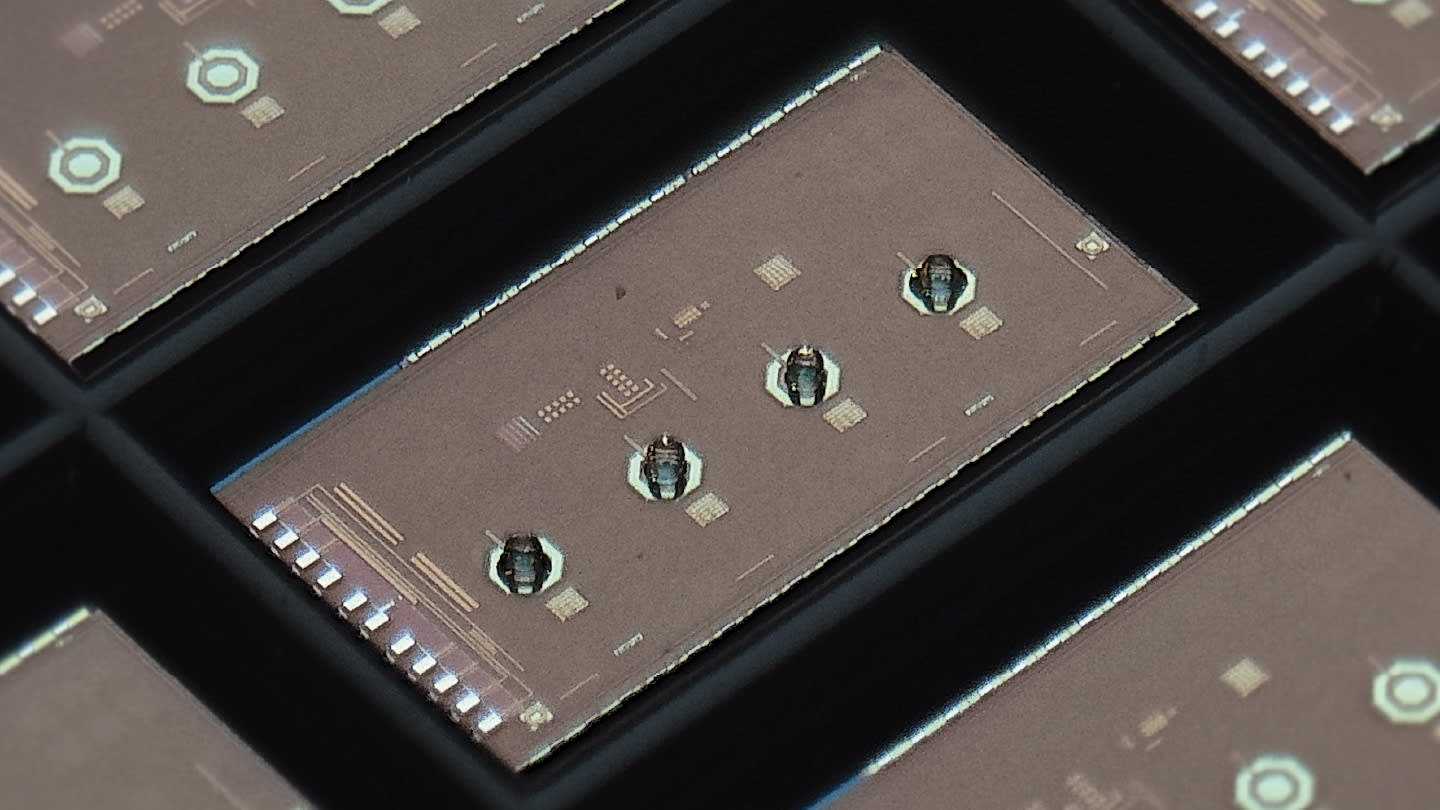
What made the difference was designing an integrated microchip system with custom electronics and microcoils built for low-power operation in live cells, and pairing it with 3D micro-printed sample holders that keep embryos perfectly aligned during measurement. It took years to optimize this into a system that delivers high-throughput and reliable results, but it’s what made this breakthrough possible.

Were there any results that surprised you?
The biggest surprise was perhaps that we saw metabolic signals predictive over morphology despite the complexity of the samples. We worked with cryopreserved cow embryos from heterogeneous sources, which introduces a lot of biological noise. Under those conditions, you wouldn’t expect clean results – yet we still found meaningful correlations with developmental success. That was a strong sign that the metabolic signature holds real potential.
When comparing embryos that developed to those that arrested, what differences in their metabolic profiles stood out most?
Lipid quantity was one clear factor: embryos lacking visible lipid signals were far less likely to develop successfully. But we also saw that peak shape mattered, suggesting differences in the structural properties of the lipids themselves.
That’s one of the unique advantages of MRS: the spectrum carries both quantitative and structural information, without any invasive labeling or staining. And importantly, MRS is highly reproducible, much more so than techniques that rely on fluorescence properties or external calibration like mass spectrometry.

How close are we to seeing micro-MRS used clinically in IVF labs – and what key hurdles need to be addressed?
We’re not there yet: the technology has not been tested on human embryos. But we are in early regulatory discussions. The core device exists, and it’s already being used for research in mammalian models. Clinical translation now depends largely on IVF labs being willing to test and support the method in a regulated environment.
I can’t disclose specific timelines or partnerships yet, but I can say this: we’re closer than people might think, and the fundamentals are in place to move forward. We believe patients will see the benefits not too far down the line.




