MS-based applications in the clinic are expanding, and the recent “BreathPrint” study suggests this reach could extend into asthma classification (1). Of seven tested volatile organic compounds (VOCs), five were confirmed as biomarkers capable of classifying asthma to the same degree as currently used tests, which typically examine induced sputum and/or blood and exhaled nitric oxide (FeNO).
Here, we speak with Jean-François (Jef) Focant to find out more.
When a patient is diagnosed with asthma, it is necessary to accurately determine the inflammatory phenotype to guide therapeutic approaches. There is not a single fully accurate test that can do this. Nowadays, clinicians use induced sputum (mucus from the lower airways) for inflammatory phenotyping. The cells present in the sputum are counted and characterized on the basis of their morphology. Based on the number of neutrophilic and eosinophilic cells present in the sputum, two thresholds have been established, and four phenotypes have been proposed, including eosinophilic asthma (high number of eosinophilic cells) and neutrophilic asthma (high number of neutrophilic cells). However, sputum analysis is not available in most medical centers. Sputum cell count can be supported or replaced by blood eosinophil count or fractional FeNO measurements, but the accuracy of these tests can still be improved. New markers are needed to support clinicians in their phenotype diagnosis – ideally using a non-invasive approach, given that a patient’s phenotype may change over time and require repeated tests.
The ‘BreathPrint’ study was accomplished in two phases. First, a set of seven potential asthma phenotyping biomarker VOCs were selected through a discovery study (276 patients) at Maastricht University in the Netherlands, using GC-Time-of-Flight MS (GC-TOFMS). Second, we performed an independent validation study (245 new patients) in Liège using GC×GC-high-resolution-TOFMS (GC×GC-HR-TOFMS). We confirmed five biomarkers that can be used to phenotype asthma with the same degree of accuracy as induced sputum, blood eosinophil count, and surrogate FeNO breathing tests. Furthermore, when blood eosinophil count, FeNO measurement, and biomarker VOCs were used together, an unprecedented classification model performance was obtained for eosinophilic asthma diagnosis. In the future, complex mixtures of biomarker VOCs could eventually improve asthma phenotyping and could become a new gold standard, next to induced sputum cell count.
Exhaled breath analysis is challenging in itself. Moreover, large-scale GC×GC-HR-TOFMS studies are not common and the analytical framework needed to be designed. First, we had to be sure that our method of sampling the breath would allow us to isolate putative biomarkers despite being present at potentially low levels amongst non-relevant exogenous molecules, while maintaining a simple sample collection procedure.
In addition, every step of the analytical workflow had to be optimized to produce high-quality data matrices to ease data processing as much as possible. Compound identification was confirmed using the two retention times, specific electronic ionization mass spectra, and high-resolution MS (HR-MS) information. Instrument performance (for example, linearity and limit of detection) was evaluated for the different targets. Sample batches included quality control standards to account for possible instrumental variations and to ensure data integrity.
The same care was applied in the optimization of the pre-processing and processing workflow optimization to ensure complete control of the analytical process. The classification models were built using random forest – a machine-learning algorithm based on a forest of decision trees. Each model was based on bootstrapping cross-validation and data splitting between training and test sets.
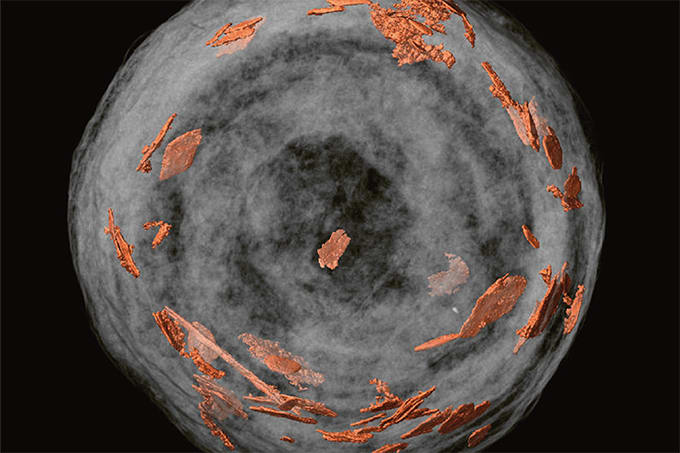
So far, we have been using GC×GC-HR-TOFMS to confirm a set of five biomarkers using a targeted approach. What we are doing now is to reconsider the entire validation set (245 patients) using a non-targeted approach. As a matter of fact, we have created a composite image template containing more than 700 analytes that can be used to highlight subtle differences in the breath fingerprint of asthmatic patients. Such a non-supervised volatilomic approach has the potential to link specific VOC profiles to subsets of patients based on a number of factors, including current medication, food habits, environment, toxicant exposure, and so on. These VOC fingerprints certainly hold a significant amount of information that could be revealed… From an analytical point of view, because of the availability of HR-MS data, we could also investigate other data-mining approaches, such as Kendrick Mass Defect classifications.
We hope that this unique approach will be positively received by the medical community, which desperately needs better ways of phenotyping asthma. We have already been duplicating selected sample measurements with selected-ion flow-tube MS (SIFT-MS) analyses to evaluate the possibility of transposing the method to simpler instrumentation that could be used directly in hospitals for the screening of the five biomarkers molecules – or to create pattern-based patient classification methods. Direct sample introduction into SIFT-MS would also help eliminate the need for the transfer procedures prior to measurement. Such a move would be the logical next step in the line of making this VOC approach usable by practitioners in the hospital environment – and perhaps even in doctor’s offices.
Time will tell. But I am quite sure that there is room for MS-based diagnostic strategies that rely on VOC patterns in the medical field. Will we see GC×GC-HR-TOFMS instruments blooming in hospitals? I’m not sure at this point. Will medical staff domesticate these complex instruments? I guess it depends if the trend goes in the direction of target analysis of validated biomarkers or towards exhaustive breathprinting of patients. In any case, current instrumentation in the GC×GC-MS domain will definitely play some role in medical diagnosis based on volatilomics in the future – and it will go far beyond breath analysis…
References
- FN Schleich et al., “Exhaled Volatile Organic Compounds are Able to Discriminate between Neutrophilic and Eosinophilic Asthma”, Am J Respir Crit Care Med (2019). doi: 10.1164/rccm.201811-2210OC.