“The future is already here; it’s just not evenly distributed” – William Gibson
Since the early 1960s, there have been more than 32,000 articles about pharmacogenomics referenced on PubMed, and almost 25,000 articles cited on pharmacogenetics. Clearly, these are not new fields of research. Yet, these studies and the advances in research tools – and the assays used with them – are not widely used in clinics.
But pharmacogenomic technologies now have the potential to improve diagnosis and treatment – and boost efficiencies within healthcare systems. How? By providing better and more efficient care for patients and offering up-to-date services for health professionals – thus meeting the needs of payers.
A few useful definitions
The terms pharmacogenomics and pharmacogenetics are frequently used interchangeably. There are, however, distinct differences.
Pharmacogenetics – a term that first entered use in the late-1950s – studies the genetic causes of individual variations in drug response. Whereas pharmacogenomics (or PGx) – a term that first began appearing in the 1990s – deals with the simultaneous impact of multiple mutations in the genome that may determine the patient’s response to drug therapy; in short, the term reflects the combining of pharmacology and genomics (1).
The purpose of PGx testing is to determine the risk of side effects and/or the likely effectiveness of a given medication. Pharmacogenomics is important for precision medicine, which aims to tailor treatment to each person or to a group of people. By identifying patients who may be genetically predisposed to severe adverse drug reactions, which are responsible for 10-30 percent of all hospital admissions in older patients (2,3) and cause over 106,000 deaths annually in the US (4) pharmacogenomics may improve patient safety – as well as improving treatment efficacy and reducing overall health care costs.
Pharmcogenomics is currently used before prescribing the antiviral drug abacavir (Ziagen) to patients with HIV (U.S. Food and Drug Administration (FDA) Section 1: Pharmacogenetic Associations for which the Data Support Therapeutic Management Recommendations). Doctors now routinely test for a genetic variant that makes a negative reaction to the drug more likely. Pharmacogenomics is also being applied in research to other therapeutic areas, such as psychotropics, cancer, pain, and cardiovascular disease.
In short, pharmacogenomics can improve lives, reduce costs, and simplify decision-making, by focusing research efforts on four aims:
- Preserving the care team’s wellbeing – by empowering healthcare providers in their treatment decisions.
- Improving quality of care – by optimizing the experience and satisfaction of patients.
- Lowering the cost of care – by reducing unnecessary medication use, ER visits, hospitalizations, and clinical errors.
- Enabling better outcomes – for overall improvement in population health and patient quality of life.
Pharmacogenomics research is already changing the treatment model of drug selection. In the future, it will be used to develop tailored drugs for a wide range of health problems, including cardiovascular disease, Alzheimer’s disease, cancer, and asthma.
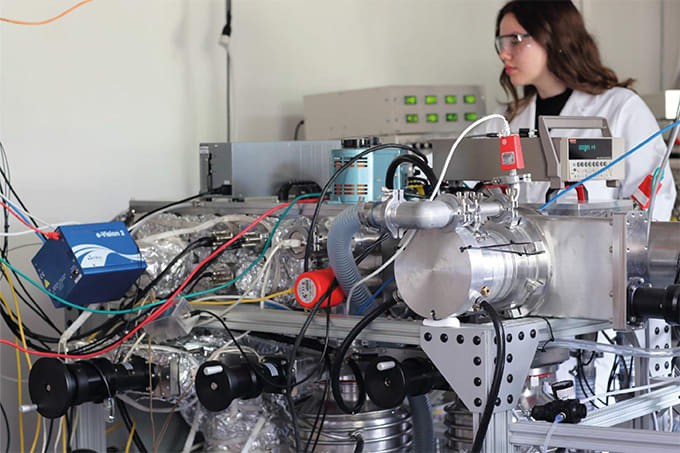
Recent advances in pharmacogenomics technologies
There are three major techniques available for pharmacogenetic panel testing: real-time polymerase chain reaction (RT-PCR), microarray, and next-generation sequencing (NGS).
RT-PCR is a molecular-biology laboratory technique that monitors the amplification of a targeted DNA molecule during the PCR – not at its end, as in conventional PCR – thus combining amplification and detection into a single step. This feat is achieved using a variety of different fluorescent chemistries that correlate PCR product concentration to fluorescence intensity. RT-PCR can identify up to 120 targets on genes and can be used quantitatively and semi-quantitatively.
Microarrays are used to simultaneously detect the expression of thousands of genes. DNA microarrays are essentially microscope slides that are printed with thousands of tiny spots in defined positions, with each spot containing a known DNA sequence or gene. Microarray solutions and customized assays are best positioned for research and development, but also preemptive analysis of all known markers. Single nucleotide variant (SNV) panels are most common.
Arguably the most exciting pharmacogenomic technology is next-generation sequencing (NGS) – a high-throughput method achieved by sequencing clonally amplified DNA templates on a massively parallel scale. NGS can identify more than 130 targets on 40 genes – looking at variants, copy number, gene expression – and employs the concept of ADME: drug absorption, distribution, metabolism. Its speed, throughput, and accuracy has helped revolutionized genetic science and given rise to an unusually wide array of clinical applications, including:
- hereditary disease detection (prenatal screening or diagnostic support)
- risk modification for common diseases (age of onset, severity, treatment strategies)
- detection and treatment strategies for circulating tumor DNA (invasive tumors and hematopathologies)
- detection of common pathogens (viral and bacterial)
- pharmacogenetic screening for dosage and treatment optimization
Moreover, NGS can identify:
- fast, slow, or intermediate metabolizers (using gene copy number)
- variations by drug and interaction pathway(s)
- varied risk across immunological, genetic, demographic (age and sex), physiological and exogenous factors and disease
- genes – currently the FDA has approved 15 genes for which the data supports therapeutic management recommendations, but more come as basic research validates the target pathways and functional variants involved
In the same patient population, NGS can, with specificity, identify those patients who will have very different responses to pharmacological treatment.
Arrays and assay panels, in concert with NGS, can be customized to add or remove targets (that are undesired), any number of targets in any genes.
Importantly, automated workflows enable quick turnaround times of one day with minimal hands-on time – compare this with older NGS technologies that could take upwards of a week.
Which technology is the best?
The “right technology” depends on the need. Key factors for lab directors to consider include:
- Turnaround time for genotyping
- Net labor costs
- Number of samples per array expected
- Cost of the array
- Content of the array
- Flexibility to adjust array content.
And clinicians should consider the following:
- Analytical validity – can the test detect the targeted gene?
- Clinical validity – does the targeted gene reliably predict disease?
- Clinical utility – does the test inform diagnosis or treatment?
What’s next for NGS?
NGS has already demonstrated myriad clinical and research applications.
Next-generation sequencing can – and will – further expand and enhance the value of pharmacogenomic research. But it’s important to know that not all NGS technologies are the same. Fortunately for healthcare systems, patients, researchers, clinicians, and pharmacists, the state of the field is continually evolving and improving.
Over time, I fully expect we’ll see the full potential of pharmacogenomics unleashed, transforming our approach to assessing risk and severity markers, optimizing treatments, and finding disease biomarkers and targets for new therapies in clinics and research labs everywhere.
References
- G Ermak, “Emerging Medical Technologies,” World Scientific (2015). ISBN: 978-981-4675-80-2
- S Royal et al., “Interventions in primary care to reduce medication related adverse events and hospital admissions: systematic review and meta-analysis,” Qual Saf Health Care, 15, 1, 23–31 (2006).
- R Thomas et al, “Pharmacist-led interventions to reduce unplanned admissions for older people: a systematic review and meta-analysis of randomised controlled trials,” Age Ageing, 43, 2, 174–187 (2014).
- J Lazarou, B Pomeranz, and PN Corey, “Incidence of adverse drug reactions in hospitalized patients: A meta-analysis of prospective studies,” JAMA, 279, 1200–1205 (1998)