Sweat is a useful biofluid in health monitoring because it contains key biomarkers and ease of access. But without active perspiration, sweat sampling is not possible. Enter Tamoghna Saha, Postdoc scholar at the University of California, San Diego, and lead researcher behind a study that pushes the limits of sweat sampling – without pushing the limits of the participant (1).
Credit: Supplied by Interviewee
How did you get into sweat research?
I always had an inclination for healthcare research, but I was introduced to “sweat”-based research during my PhD at North Carolina State University under Orlin Velev and Michael Dickey in 2017. During this time, it was standard to develop wearable prototypes that could simply measure and showcase a biomarker signal, without much note on why, how, or what physiologically led to that response. Additionally, many researchers faced challenges associated with exercise-induced sweat – biomarker dilution from excessive sweating, inability to conduct long-term monitoring, and preclusion of patients for whom exertion was contraindicated. Because of this, measuring biomarkers continuously from sweat in patients at rest was unimaginable.
This is where my research kicked in; I began investigating ways to harvest sweat non-invasively at rest. Eventually, this led me to explore whether continuous biomarker detection could also be achieved.
How did you solve the problem of harvesting sweat under rest conditions?
The fascinating part about sweat (thanks Mother Nature!) is that it is continuously released on the surface of the skin. It may not be visible due to evaporation, but I conducted a simple experiment to prove it's there – rubbing a commercial colorimetric lactate strip on my forearm and treating it with an assay. The corresponding color change proved my theory, but would this happen with other biomarkers? This increased my curiosity as to whether we could somehow extract “invisible” sweat with a pump from the skin's surface and route it through a channel for continuous collection.
We decided to deploy hydrogels as the skin pumping source and use the osmotic pressure difference between the hydrogel and sweat to facilitate sweat transport (2). Hydrogels are soft materials containing 70-80 percent water and have been extensively used in various biomedical applications. However, if you forcefully perturb the solute–solvent equilibrium (via treatment with a concentrated solution) and force encounter with a solvent-rich source (such as sweat inside skin), it will take up more solvent through sweat and biomarkers to go back to its equilibrium state. This concept was first attempted on a benchtop setup and then implemented onto skin.
Once the sweat is extracted, the next step is to sample it. We used paper as the sweat transport media thanks to its inherent hydrophilic nature, convenience to access and design, and capability to support fluid flow via capillary wicking (3).
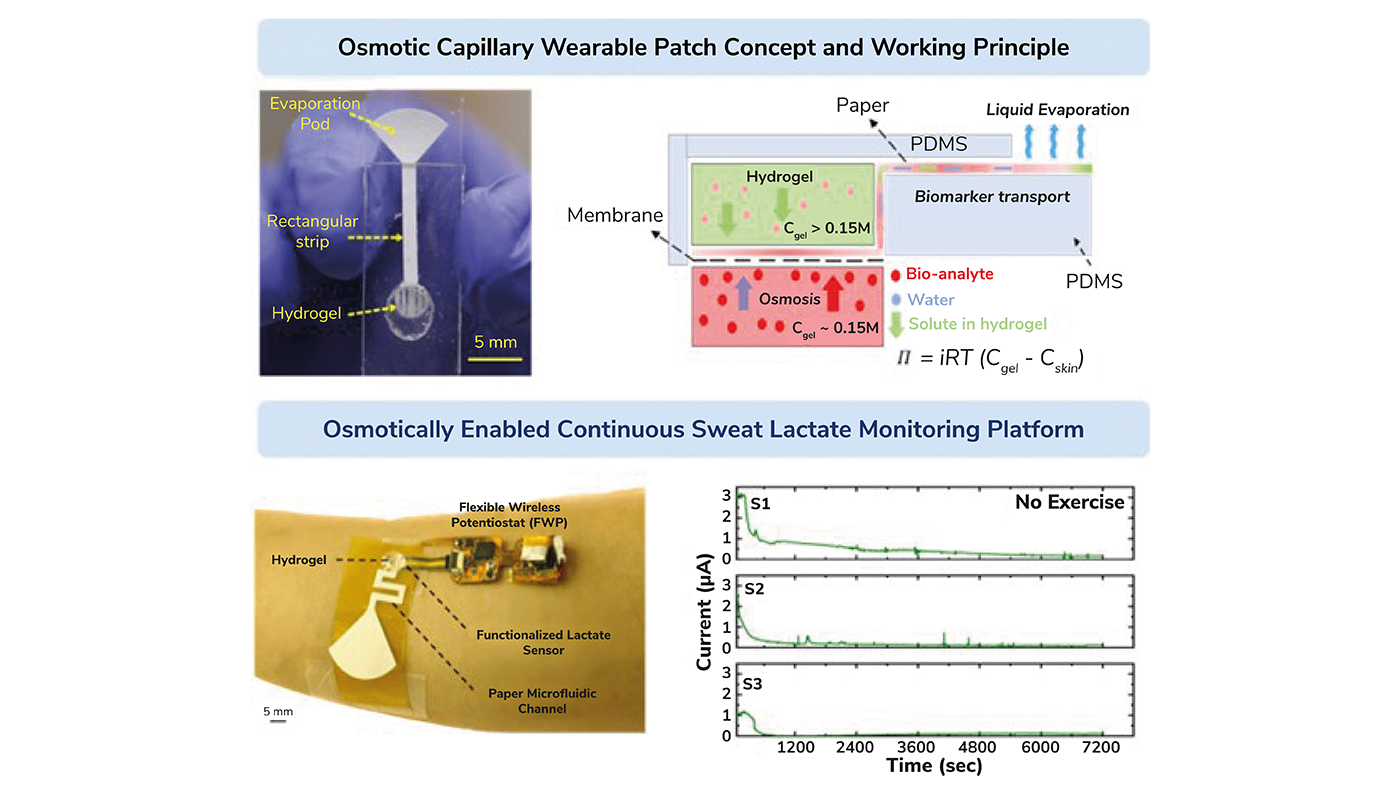
[Figure 1. Top row: (Left) Our first wearable sweat sampling prototype based on the osmotic capillary principle and its (Right) working mechanism schematic. Bottom row: (Left) A prototype functioning on osmotic capillary principle for continuous sweat extraction and lactate sensing. (Right) Temporal sweat lactate response from three subjects at rest. Credit: Tamoghna Saha]
What other challenges did you face during your research process?
Osmotically extracted sweat brings a multitude of challenges. Firstly, the process is relatively slow, with at least 15–30 minutes of initiation time. The hydrogel’s pumping capability and the on-body location also dictates this timeline due to varying sweat gland density (4). Secondly, the volume of extracted sweat is low by a few hundred nL/min and doesn’t have enough pressure to be routed through a conventional polymeric microfluidic channel. Hence, we introduced the paper channel to overcome this issue. And finally, there are issues with hydrogels drying overtime if they aren’t sealed properly or treated with low volatile solvents, such as glycols (5).
What was the role of sweat lactate in your study?
Lactate is an indicator of oxidative stress (exertion) and muscle health. Let's take an individual who doesn’t work out frequently but decides to play soccer one day. Initially, their performance will be good as oxygen is properly utilized by blood, but will soon start to reduce with fatigue accumulation and a low supply of oxygen to the blood. To keep performance levels up, the body will continue to burn glucose through a non-oxygen supported pathway which will eventually increase lactate production in the body. This is why a quicker and greater appearance of elevated lactate levels in the blood is a sign of poor physical performance. Such elevated parameters are critically investigated to determine the optimal performance of athletes.
In our research, we decided to show lactate extraction with our osmotic system as residual lactate is always present on the skin surface and its concentration in sweat is relatively high compared with other sweat metabolites measured in millimolar ranges (6). Our wearable system used polyacrylamide hydrogels for 2 hours of sweat lactate extraction from the forearm region, which was validated with both colorimetric and electrochemical detection techniques. During this time period, we sampled 6-7 µL’s of sweat on the paper channel before extracting the lactate via centrifugation and quantifying it with a colorimetric assay. Colorimetry can only provide the cumulative amount of the sampled lactate, which meant that, to get real-time continuous trends, we needed to separately develop an enzymatic electrochemical sensor and interface it to the paper fluidic pathway. It was very important to place the sensor close to the inlet hydrogel spot to reduce the response lag-time under low sweat rates. This allowed us to view lactate signals within 20–30 minutes.
After testing our system under exercise, we came across two conclusions. Firstly, a medium intensity exercise with 50–60 percent of maximum heart rate (MHR) is the best zone to estimate peak sweat lactate concentration. This is because the rate of lactate appearance in sweat is proportional to the rate of sweat release. However, blood lactate concentration doesn't show a significant increase.
Our second conclusion of this test identifies that high intensity exercise with over 80 percent MHR dilutes the sweat lactate concentration but elevates blood lactate concentration. This is because more water is released in sweat than lactate and the individual's “lactate threshold” is surpassed. As with the first conclusion, there is also no positive correlation observed. The osmotic effects get minimized with exercise since active sweat majorly contributes to the lactate in the patch.
What does this research mean for future personalized healthcare?
Osmotic based sweat extraction has the potential to revolutionize personalized healthcare. This concept supports non-invasive and exertion free health monitoring from sweat, which not only benefits healthy individuals, but also neonates and elderly patients. Currently, this concept has only been established for sweat lactate in healthy individuals, but other biomarkers on different subjects under varying physiological conditions will be investigated.
Our technique fundamentally focuses on the “biofluid sampling” concept from skin and could be integrated with soft microneedle patches for continuous interstitial fluid sampling. We have a patent application for this research, so stay tuned for developing outcomes! ASSIST and UC San Diego’s websites are continuously updated with upcoming translational wearable technologies.
References
- T Saha et al., ACS Appl. Mater. Interfaces, 13, 7 (2021). PMID: 33587589.
- T Saha et al., ACS Sens, 7, 7 (2022). PMID: 35820167.
- T Shay et al., Biomicrofluidics, 14, 3 (2020). PMID: 32566070.
- T Shay at al., Lab Chip, 4 (2017). PMID: 28150821.
- T Saha et al., Lab Chip, 24 (2024). PMID: 38197332.
- Patent Application Publication “Functioning of interstitial fluid harvesting and processing patch using gel osmosis and paper microfluidics” (2023). Available at: https://bit.ly/3vHM7iY.




