Precision Medicine 2050: With Lingjun Li
In the future, AI-assisted diagnostic tools could analyze your health status and prescribe personalized interventions tailored exactly to your biology – but not until we can better detect biomarkers at extremely low concentrations
James Strachan | | 12 min read | Interview
Imagine a world where a simple drop of blood, a finger-prick, or a wearable sensor provides a continuous readout of your biological health – without having to visit the hospital. Where AI-powered tools analyze not just your DNA, but your entire molecular profile, to predict risks, guide personalized treatments, and even prevent diseases from developing at all. What would it take to make this vision a reality? What role will analytical science play? And can we get there by 2050?
Here, as part of a series of articles tackling these important questions, we speak with Lingjun Li, Vilas Distinguished Achievement Professor of Chemistry and Pharmaceutical Sciences, Charles Melbourne Johnson Distinguished Chair in Pharmaceutical Sciences, School of Pharmacy and Department of Chemistry, University of Wisconsin-Madison, USA.
Lingjun Li
Has the Human Genome Project realized its precision medicine potential?
The Human Genome Project has certainly brought major advancements, particularly in understanding gene mutations and their role in disease. Mutations in genes like RAS, for example, have been implicated in different cancer types. But while the genome provides a blueprint for biology, it’s the proteins and protein complexes that actually carry out the functions in a cell.
Genes alone don’t always tell us the whole story. Many factors influence how genes are expressed, including protein translation and post-translational modifications. For instance, phosphorylation plays a major role in regulating protein function, and in our lab, we also study protein glycosylation, citrullination, and other modifications that alter protein structures and activities. These modifications can serve as critical biomarkers that aren't always evident from just looking at the genome.
There are also proteoforms to consider – the idea that a single gene can give rise to 20, 30, or even more different protein variants. This adds another layer of complexity to biology that isn’t captured at the genetic level.
Beyond proteomics, there’s growing interest in other omics fields. Metabolomics gives insight into molecular phenotypes, while lipidomics has gained traction in disease research. In our lab, we’ve begun studying lipid structures in even more detail – looking not just at their composition but also at finer structural details like double bond positions and stereochemistry. These subtle differences could provide new insights into disease mechanisms that were previously overlooked.
Many diseases are incredibly complex, and no single omics approach can fully capture them. A multi-omics strategy – combining genomics, proteomics, metabolomics, and lipidomics – offers a more comprehensive understanding of disease states and could be key to advancing precision medicine.
When did we fully realize that we’d need to go beyond the genome?
I think the concept of the proteome really started gaining attention around 1995 when the term was first coined. At that time, people were beginning to understand the complexity of post-translational modifications (PTMs) on a global scale, but the ability to study them in depth was still quite limited.
A major turning point came with advancements in analytical science, particularly in mass spectrometry. The improvements in sensitivity, throughput, and chemical specificity allowed us to start mapping site-specific modifications in proteins and truly appreciate the molecular complexity of the proteome.
A lot of what we’ve learned in the past two decades has been enabled by technology – better instrumentation, improved sampling techniques, and more powerful computational tools for data analysis. These advancements have not only transformed proteomics but also helped expand other fields like metabolomics and glycomics, which focus on different layers of molecular regulation.
Can you expand on the role of analytical science in delivering a precision medicine future?
When we talk about translating discoveries into clinical settings, there are a few key challenges.
First, in biomarker discovery, we often use high-end mass spectrometry in academic labs to identify potential markers. But for these biomarkers to be clinically useful, we need large-scale validation in diverse patient cohorts. This requires robust, reproducible, high-throughput methods that are also affordable enough to be used in a hospital or diagnostic lab – which is very different from an academic research setting.
Right now, ELISA assays are widely used in clinical diagnostics because they are simple, scalable, and cost-effective. But translating mass spectrometry-based discoveries into clinical practice requires methods that can bridge the gap – such as the use of triple quadrupole mass spectrometers or multiple reaction monitoring (MRM)-based assays, which are more targeted and reproducible than discovery-based proteomics.
Another challenge is making mass spectrometry itself more clinically viable. There are emerging technologies, like mass spectrometry-based point-of-care devices (e.g., the MasSpec pen), which could make real-time, in-clinic proteomic and metabolomic analysis a reality. But for widespread clinical adoption, we still need to simplify the workflows, reduce costs, and improve automation so that these technologies can be routinely used in diagnostics.
The Single-Cell Solution
What role could single-cell omics play in precision medicine?
With Lingjun Li
Cells are the fundamental functional units of biological systems. If we want to truly understand biological processes, we need to study them at the single-cell level.
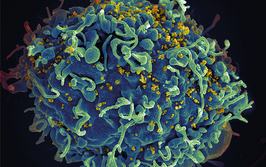
Take cancer, for example – the tumor microenvironment is highly heterogeneous, and tumor development often starts from a single cell. If we can identify small populations of abnormal cells, or even detect the earliest molecular changes in a single cell before it becomes cancerous, we can improve diagnostics and treatment strategies.
Another great example is in neurology. My lab studies neurobiology of model organisms and neurological diseases, and we see how neighboring neurons can use vastly different neurotransmitters and neuropeptides to communicate. When diseases like Alzheimer’s or Parkinson’s occur, these molecular compositions change, and being able to analyze neurons at the single-cell level will help us understand how these diseases progress. Even small differences in lipid composition or protein modifications – like phosphorylation – between adjacent neurons can have a major functional impact.
Another area where single-cell omics is expanding rapidly is spatially resolved omics. Nature Methods recently named spatial proteomics as the Method of the Year, which speaks to its growing significance. Spatial omics allows us to map molecular compositions within individual cells, helping us understand cell-to-cell interactions in ways we couldn’t before.
For example, in cancer metastasis, tumor cells interact with neighboring cells in complex ways, influencing disease progression. Similarly, in organoids, we see how different cell types interact in an artificial system. These kinds of studies will transform our understanding of both disease mechanisms and therapeutic interventions, making single-cell omics a critical part of the future of precision medicine.
We’re essentially working toward creating region- and cell-type-specific molecular atlases – whether that’s for the brain, the heart, or other organs. There are already major initiatives working on this, like HuBMAP (Human Biomolecular Atlas Program) and other large-scale multi-omics efforts that aim to build comprehensive molecular maps of different organs. But ultimately, the goal is to get down to a single-cell, cell-type-specific resolution – to truly understand what’s happening both in healthy states and in disease conditions.
I also think that as technology advances, we’ll be able to investigate post-translational modifications (PTMs) and PTM crosstalk at the single-cell level. This will be incredibly powerful and informative, because PTMs are essential for cell signaling and function, and they play a crucial role in disease progression.
If we can integrate this multi-omic data with high-resolution imaging and spatial proteomics, it will transform how we approach both biomarker discovery and drug development. We’ll not only be able to better predict disease but also design more precise therapies that directly target disrupted signaling pathways at a molecular level.
In the next few years, I expect to see: more comprehensive single-cell molecular atlases across different organ systems; advances in spatial proteomics and single-cell PTM analysis for deeper biological insights; and better integration of multi-omics data, leading to more targeted and effective therapeutics. It’s a very exciting time for single-cell research – and precision medicine.
Is the bigger issue on the instrumentation side – meaning we need better tools to deliver high-throughput assays – or is it more about applying existing technologies in better ways?
I think the challenge is really twofold. First, on the instrumentation side, we still need more sensitive instruments. Even though we've made great advancements, when it comes to diagnostics – especially for conditions like cancer or neurodegenerative diseases – our current instruments are not sensitive enough. We need instruments that offer: higher resolution and sensitivity, better ion transmission efficiency in mass spectrometry, and reduced analyte bias and suppression, so we can detect a broader range of compounds without having to fine-tune the instrument differently for different analytes. Another major instrumentation challenge is sample preparation. If we want to scale down analyses to single-cell resolution, we need better micro-scale sampling techniques that can seamlessly integrate into high-throughput workflows.
Second, on the data analysis side, we face enormous challenges in computational tools and integration. If we truly want to leverage multi-omics approaches, we need: more powerful AI and machine learning algorithms to process and interpret vast datasets, better strategies to integrate different omics layers (genomics, transcriptomics, proteomics, metabolomics, etc.) into meaningful clinical insights, as well as scalable bioinformatics pipelines that can handle the complexity of precision medicine.
How could analytical science help shift healthcare towards a more preventative approach?
Longitudinal tracking of global proteomic changes could be hugely valuable for early disease detection and preventive medicine.
In our research, we’ve been working on Alzheimer’s disease biomarker discovery, looking at cerebrospinal fluid (CSF). However, since spinal taps are invasive and not ideal for routine clinical use, we’re also investigating blood-based markers – in plasma or serum – to see if they correlate with CSF findings. Blood-based assays would make long-term, global proteome monitoring much more feasible for clinical applications.
Another major aspect of this is tracking post-translational modifications (PTMs) over time. We’ve been particularly focusing on glycoprotein and glycan changes – which are known to be highly relevant to aging and disease progression. Many diseases, including neurodegenerative disorders, are age-related, so distinguishing normal aging-related changes from early disease markers is crucial.
If we could monitor a person’s proteome longitudinally, we could build a baseline for what’s “normal” for them and detect subtle deviations that indicate early disease risk. Right now, when we analyze proteomic changes, it’s often difficult to separate the effects of aging, sex, diet, and lifestyle from actual disease-specific changes. But with long-term, global-scale omics tracking, we could pinpoint specific markers that truly reflect disease progression, rather than just general physiological variation.
Beyond proteomics, lipidomics and metabolomics are also gaining interest in this space. Lipids and metabolites are highly dynamic and strongly influenced by environmental factors like diet, lifestyle, and stress, making them valuable indicators of health and disease. Integrating multi-omics profiling over time could help us create a much more complete picture of an individual’s health trajectory and enable more personalized interventions before disease onset.
Thinking “big picture” – let’s say 2050 – what might precision medicine look like?
In a dream scenario, a visit to the doctor (or even an at-home health check) could involve a simple drop of blood or another biofluid sample, and within minutes – AI-assisted diagnostic tools could analyze your health status and prescribe personalized treatments tailored exactly to your biology.
Imagine a system where continuous health monitoring is effortless – perhaps through non-invasive wearables, or small, routine biofluid tests that allow real-time tracking of health markers. If early signs of disease appear, customized interventions – whether it’s medication, lifestyle changes, or preventive therapies – could be immediately recommended based on your unique molecular profile.
The ultimate goal would be to replace the reactive "treat the disease" model with a proactive, preventive healthcare system. Instead of waiting until a disease reaches critical stages, precision medicine could identify risk factors early, allowing early intervention – potentially preventing diseases from developing altogether.
This vision of highly personalized diagnostics and treatment plans would revolutionize healthcare, making it more effective, more accessible, and more tailored to each individual – and that would truly be the dream of precision medicine.
And what do you think is the biggest barrier to achieving this vision of precision medicine?
I would say that right now, our technology is not quite there yet. While we've made tremendous advancements, there are still major challenges – especially in detecting early disease markers with the required sensitivity.
For example, blood samples are highly complex, and when we talk about early diagnostics, we need technologies that can detect biomarkers at extremely low concentrations. Right now, many assays still lack the sensitivity and robustness needed to reliably catch early disease signals. That’s why a lot of research is focused on affinity enrichment strategies – especially for post-translational modifications, which are often key to understanding disease states.
Another major challenge is single-cell analysis – it’s an incredibly powerful approach, but we still struggle with reproducibility, robustness, and scalability. The technology needs to mature before it can be fully integrated into clinical workflows.
Then, of course, funding is a big factor. Developing newer, more sensitive generations of instrumentation is very expensive, and requires sustained investment. Research labs can push scientific frontiers, but without adequate funding, it’s difficult to translate these innovations into affordable, widely accessible clinical solutions.
And finally, healthcare affordability is a critical issue. Even if we develop breakthrough technologies, will they be cost-effective enough to be widely adopted? Will healthcare systems be willing to cover these advanced diagnostic assays?
That said, I do think the future is bright. There’s so much to do, but I truly believe that multi-omics is the way forward.

Over the course of my Biomedical Sciences degree it dawned on me that my goal of becoming a scientist didn’t quite mesh with my lack of affinity for lab work. Thinking on my decision to pursue biology rather than English at age 15 – despite an aptitude for the latter – I realized that science writing was a way to combine what I loved with what I was good at.
From there I set out to gather as much freelancing experience as I could, spending 2 years developing scientific content for International Innovation, before completing an MSc in Science Communication. After gaining invaluable experience in supporting the communications efforts of CERN and IN-PART, I joined Texere – where I am focused on producing consistently engaging, cutting-edge and innovative content for our specialist audiences around the world.