Only Gene Deep
Advances in genomics are certainly thrilling, but let’s not forget that a tumor is more than a bundle of genetic information.
Han van Krieken |
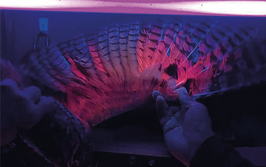
As histopathologists, we try to understand disease by looking at tissues. We see a snapshot of cells in their tissue environment. We can see whether they are normal or abnormal, whether there are too many or too few cells, how they are organized and how they interact. We can localize enzymes and proteins, measure expression levels, determine DNA alterations, and so on – and by bringing all this knowledge together, we can form a fairly complete picture of the disease that manifests itself in the tissue. These efforts provide the patient and the treating physician with information that can be used to choose the best possible treatment (or no treatment).
In this era of genetics, we are increasingly able to sequence the DNA of individuals and tumors, which allows us to quickly diagnose many different diseases that are caused by changes in genes, such as cystic fibrosis or Noonan syndrome. For cancers, we get information on the gene alterations that drive the tumor; for example, c-Erb2 amplification or ALK-fusions. Increasingly, it is suggested that whole genome sequencing will replace traditional forms of diagnosis. Indeed, if a child with an intellectual disability comes for a diagnosis, physical examination is already replaced by DNA analysis. And I was informed that in Hong Kong, where the incidence of EGFr mutated lung cancer is quite high compared with western countries, lung cancer is already diagnosed using genetic tests on blood samples in patients with inaccessible pulmonary lesions; if an EGFr mutation is found, it is regarded as sufficient evidence that the patient should be treated using an anti-EGFr approach. But in my view, although sequencing is an important diagnostic tool with much potential, it will never give the complete picture.
An example: it was recently shown that the cells within a tumor the size of a ping-pong ball will carry a total of 100 million mutations, with only a few of those mutations present in the majority of cells (1). Not only does this finding indicate that tumor heterogeneity on the cellular level is enormous, but also that complete sequencing of tumors provides us with so much data that it becomes useless. Quite interesting, of course, but not surprising for pathologists. In fact, that the nuclei in cancer cells are extremely variable compared to normal cells has been one of the most important criteria a pathologist uses when making a diagnosis of cancer for more than a century...
Furthermore, a tumor consists of not only neoplastic cells but also stromal cells, such as fibroblasts, inflammatory cells, endothelial cells and others. There is enormous variation in the ratios of these cell types between tumors – variation that has been shown to relate to treatment response and survival of the patient. Such variation cannot be found by sequencing the tumor or even the germline DNA.
Genes act through proteins, but proteins are not only modified by genetic mechanisms. Indeed, proteomic approaches are likely to give even more information, but replacing genomics with proteomics (which will take quite some time) will also not tell the whole story. Cells and tissues are so complex that we cannot fully understand what is going on by extracting only the genes and proteins. Spatial orientation, communication between cells, composition of tissues are all critical.
To that end, analyzing tissues with the microscope will remain an extremely cheap and fast way of providing useful information. But I am also convinced that we can benefit from new approaches in this field to extract even more information; for instance, deep-learning approaches – where standard tissue image analysis is supplemented with new information based on automated quantification of structures and protein levels – have great potential.
Of course, sequencing of tumors has given us a lot of valuable information – and will continue to do so – but we must remember that many other factors are equally important. As we all know, we are more than our genes – and a tumor is more than its genetic make-up.
- S Ling et al, “Extremely high genetic diversity in a single tumor points to prevalence of non-Darwinian cell evolution”, Proc Natl Acad Sci USA. 112: E6496-505 (2015). DOI: 10.1073/pnas.1519556112. Erratum in: Proc Natl Acad Sci USA, 113: E663 (2016). PubMed PMID: 26561581
A pathologist with special expertise in gastrointestinal and hematopathology, Han is immediate past President of the European Society of Pathology, the chair and department head of pathology at Radboud University Medical Center in Nijmegen, as well as co-chair of the RadboudUMC Center for Oncology. He chose to enter pathology because of the intellectual challenge and the huge impact pathologists have on patients’ wellbeing, and says that the highlight of his career was “the discovery that mantle cell lymphoma is a distinct entity that can be easily diagnosed using cyclin D1 staining.”