Precision Medicine 2050: With Rob Monroe
The next installment in our series of articles exploring analytical science’s role in delivering a precision medicine future, Leica’s Rob Monroe explains why he’s excited about higher resolution diagnostics
| 6 min read | Interview

Imagine a world where a simple drop of blood, a finger-prick, or a wearable sensor provides a continuous readout of your biological health – without having to visit the hospital. Where AI-powered tools analyze not just your DNA, but your entire molecular profile, to predict risks, guide personalized treatments, and even prevent diseases from developing at all. What would it take to make this vision a reality? What role will analytical science play? And can we get there by 2050?
Here, as part of a series of articles tackling these important questions, we speak with Rob Monroe, Chief Medical Officer for Leica Biosystems and Chief Scientific Officer, Oncology, for Danaher Diagnostics.
What does precision or personalized medicine mean to you?
Precision or personalized medicine means delivering the right treatment to the right patient at the right time. With respect to pathology and lab medicine, precision medicine typically involves the assessment of biomarkers of disease to determine which therapies would be best suited for a specific patient. The most well-established use case for personalized medicine to date is oncology, where a variety of therapeutics have been designed to target specific features of tumors, such as mutations in key genes or overexpression of critical proteins.
At a broader level, precision medicine involves a more holistic assessment of the patient, including demographics (i.e., age, sex, race), past medical history, comorbidities, genetics/pharmacogenetics, and other factors that could potentially impact the choice and efficacy of a specific treatment. True personalized medicine takes all of this information into account in selecting and tailoring therapy for individual patients.
What big health challenges could be tackled using a precision or personalized medicine-based approach?
Outside of oncology, most drugs are still being delivered to patients without selection in a “one size fits all” approach, irrespective of biomarker status. This state of affairs presents the healthcare system with a major opportunity to improve patient outcomes while simultaneously reducing costs by supporting the development of companion diagnostics across therapeutic areas.
Within the field of oncology, one of the major issues going forward is the approval of multiple therapeutics for the same indication and the associated challenge of selecting which one to give to the patient. Higher resolution diagnostics have great potential to address this challenge through more precise and quantitative biomarker assessments that can be translated into more accurate prediction of patient response and selection of the therapy with the highest probability of success.
Can you give an example or two of precision or personalized medicine in action?
The classic example of personalized medicine goes back about 25 years to the early days of therapeutic antibodies. Breast cancer patients with overexpression of the HER2 protein were found to be highly responsive to treatment with a monoclonal antibody called Trastuzumab. This led to the approval of Trastuzumab for patients with high levels of HER2 as determined through a companion diagnostic immunohistochemistry assay. This approach to patient selection for Trastuzumab while still in use today has evolved as new drugs, specifically antibody-drug conjugates that target HER2, have recently been approved that are effective in treating patients with lower levels of HER2, requiring identification of so-called “HER2-low” expressors.
Another example of personalized medicine in action is the assessment and targeting of driver mutations in the treatment of lung cancer. Genomic testing of lung cancers with PCR or NGS assays has become standard of care at the time of initial diagnosis to identify targetable genomic alterations including mutations and gene fusions in genes like EGFR and ALK. Lung cancers with specific mutations in EGFR are treated with small molecule inhibitors such as erlotinib while those with gene fusions involving ALK are treated with ALK inhibitors such as crizotinib.
What might precision medicine look like in the future?
In the future, personalized medicine will extend beyond cancer to other diseases. We will increasingly see the application of precision medicine to patients with autoimmune, inflammatory, metabolic, cardiovascular, and neurodegenerative diseases through the development of biomarkers that identify responders and non-responders in these patient populations.
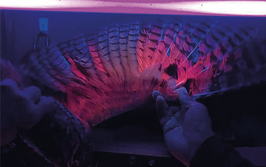
Within oncology, we're likely to see an evolution in the technologies used for patient selection. More accurate, higher resolution, and higher-plex technologies will identify patients not only for single-agent therapeutics but also combination therapies that target multiple biomarkers. This evolution will require continued innovation in diagnostic approaches to allow for the simultaneous evaluation of multiple biomarkers in the same assay to predict, for example, which ADC or combination therapy is most appropriate.
Can you expand on the role of analytical science / analytical technology in the future of precision medicine?
The future of precision medicine will be shaped by advancements across the field of analytical science. In particular, next generation sequencing and CRISPR-based systems will profile patients’ genomes to predict their likely response to treatments; mass spectrometry and chromatography will support precision medicine though superior analysis of biomarkers; and AI driven technologies will identify patterns in complex data sets to help clinicians optimize treatment plans.
What would be the ultimate goal to achieve by 2050?
The ultimate goal is for diagnostics to guide precision medicine for all drugs and therapeutic decisions. This goal extends from oncology into the other major disease areas mentioned previously, including neurodegenerative and inflammatory diseases. We're in the early days of figuring out which drug is likely to work best on which patient, but there's tremendous potential to extend the oncology paradigm to therapeutics across a range of human diseases by 2050. A related goal as we look toward 2050 is the development of diagnostics that can identify diseases like cancer and Alzheimer’s at the very earliest stages when personalized therapeutic approaches can halt progression, reverse the course, or even cure these diseases before they become problematic.
How can companies like Leica Biosystems help make precision medicine a reality?
Companies like Leica Biosystems can continue to partner with pharma companies to support the development of increasingly higher resolution companion diagnostics by leveraging multiplex technology, spatial approaches, computational pathology and AI in conjunction with new cancer therapies to more accurately select patients for these treatments.
Any final thoughts on the future of precision medicine?
Precision medicine has the potential to make a dramatic impact across the spectrum of human diseases, improving patient care while reducing costs through earlier detection of disease and more accurate patient selection.